eye Insights Issue 01: Ocular Trauma
 Staying Boston Strong! Improving ophthalmic disaster readiness and response planning.
Staying Boston Strong! Improving ophthalmic disaster readiness and response planning.
|
Focus on Ocular Trauma • Key Lessons Learned • Benchmark protocols for managing open-globe repairs April 15, 2013: Residents, fellows and faculty from Mass. Eye and Ear and Harvard Medical School (HMS) clinical affiliates and Boston Medical Center at Boston University coordinated efforts to provide ocular trauma care to victims of the Boston Marathon bombings.
|
Editor-in-Chief: Joan W. Miller, MD, FARVO
Managing Editor: Matthew F. Gardiner, MD
Communications Director: Suzanne Ward
Clinical Advisory Group: Carolyn E. Kloek, MD, Deeba Husain, MD, Ankoor S. Shah, MD, PhD, Angela V. Turalba, MD
Browse all issues > > | Email: eyeinsights@meei.harvard.edu
| eye Insights 1 PDF | 599 KB |
Focus on Ocular Trauma
Dear Colleagues,
Welcome to our first issue of Eye Insights, Mass. Eye and Ear’s clinical practice newsletter for Ophthalmologists. Eye Insights offers busy physicians practical and relevant best practice information from Mass. Eye and Ear specialists covering a wide range of ophthalmic diseases and conditions.
Our first issue focuses on Ocular Trauma and includes our benchmark protocols for managing open-globe injuries and minimizing the risks of endophthalmitis after surgical repair. We have provided key recommendations from a report prepared by ophthalmology faculty from Harvard Medical School and Boston University who were involved in emergency response efforts following the Boston Marathon bombings; a paper is in press at the journal, Ophthalmology. This report also provides important insights and valuable lessons in disaster-readiness and response planning.
We hope you find Eye Insights to be a helpful tool for supporting your patient management practices. The newsletter will be mailed twice a year in spring and fall, and back issues will be available online.
Sincerely,
Joan W. Miller, MD, FARVO
Chief & Chair, Department of Ophthalmology
Massachusetts Eye and Ear, Massachusetts
General Hospital, Havard Medical School
Key Lessons Learned from the Boston Marathon Bombings
Key Lessons Learned from the Boston Marathon Bombings5
- Promote use of eye shields on the scene for patients with potential eye injuries
- Maintain reliable communications
- Deepen the ophthalmology call algorithm
- Integrate ophthalmology services into trauma teams and maintain a voice in hospital-wide disaster planning
- Provide patients with replacement spectacles ASAP during response efforts
5 Ocular Blast Injuries in Mass-Casualty Incidents: the Marathon Bombing in Boston, Massachusetts and the Fertilizer Plant Explosion in West, Texas [In press, Ophthalmology 2014], Yoshihiro Yonekawa, MD, et al.

Benchmark Protocols for Managing Eye Trauma
Epidemiology
The annual incidence of open-globe injuries worldwide is estimated to be 203,000 cases. Overall, males comprise approximately 80 percent of open-globe injuries. Males age 10 to 30 are at greatest risk. The chance of blunt globe rupture also increases after some types of ocular surgical procedures, including: large incision cataract removal, cornea transplant, glaucoma filtering, or refractive surgery.
Standardized Terminology2
| TERM | DEFINITION |
| Open-globe injury | Full-thickness wound of eye wall |
| Laceration | Full-thickness wound of the eye wall, caused by a sharp object |
| Lamellar laceration | Partial thickness wound of the eye wall |
| Rupture | Full-thickness wound of the eye wall, caused by a blunt object |
| Penetrating injury | Only entrance wound is present |
| Perforating injury | Both an entrance and exit wound are present |
2 Ferenc Kuhn, Robert Morris, Viktória Mester, C. Douglas Witherspoon, “Terminology of Mechanical Injuries: The Birmingham Eye Trauma Terminology,” in Ferenc Kuhn Ocular Traumatology (Springer-Verlag Berlin Heidelberg 2008), 3-12.
Eye Injury Zones
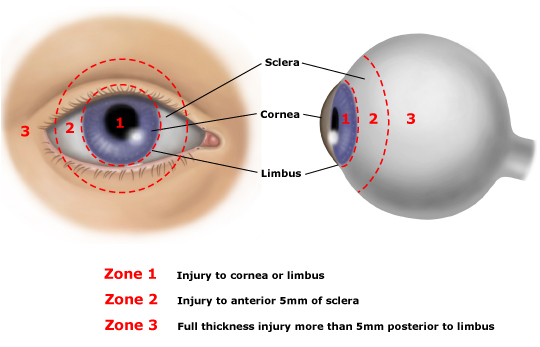
Reproduced with permission from: Andreoli CM, Gardiner MF. Open globe injuries: Emergent evaluation and initial management. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (Accessed on April 9 2014.) Copyright © 2014 UpToDate, Inc. For more information visit www.uptodate.com.
Rapid Overview of Open-Globe Injury Protocol
Based on Mass. Eye and Ear’s experience, we recommend that institutions adopt a standardized management protocol for treating open-globe injuries that consists of a dedicated eye trauma service and 48 hours of intravenous antibiotics.
|
Preferred Imaging Modality:
Axial and coronal CT of the eye without contrast, utilizing 1 to 2mm cuts through Note: Ocular CT has limited ability to demonstrate an occult open-globe injury and should not be used as the sole determining factor for decisions regarding surgical exploration. |
- Ensure nothing by mouth (NPO)
- Make sure patient has been examined and cleared for life-threatening or systemic injuries
- Avoid high dose ketamine if rapid sequence induction (RSI) is required
- If RSI is necessary, rocuronium is preferred to succinylcholine for muscle relaxation
- Do not remove any protruding foreign bodies until under controlled conditions in an OR
- Avoid eye manipulation that may increase the risk of extrusion of intraocular contents
- Use a new bottle when administering eye drops to patient to ensure drops are sterile
- Place eye shield after initial eye examination
- Put patient on bed rest with head of bed elevated to 30 degrees if hemodynamic condition allows
- Treat nausea and vomiting aggressively (e.g., ondansetron 0.15 mg/kg per dose, up to 12 mg intravenously)
- Provide sedation, as needed (e.g., lorazepam 0.05mg/kg, maximum initial dose: 2 mg)
- Provide analgesia (e.g., IV fentanyl [1mcg/kg per dose, maximum initial dose: 100 mcg] or morphine [0.1 mg/kg per dose, maximum initial dose: 10 mg]
-
Begin IV antibiotics (Transfer of patients with ruptured globes to a tertiary trauma center should not delay the administration of antibiotics.):
- Vancomycin (15 mg/kg IV, maximum dose: 1.5 grams)
- Ceftazidime (50 mg/kg IV, maximum dose: 2.0 grams)
- Fluoroquinolone for penicillin allergic patients (e.g., ciprofloxacin 10 mg/kg IV, maximum dose: 400 mg, use with caution in patients under 18 years of age) - Urgent surgical repair, ideally within 24 hours of injury
Keeping Endophthalmitis Rates Near Zero
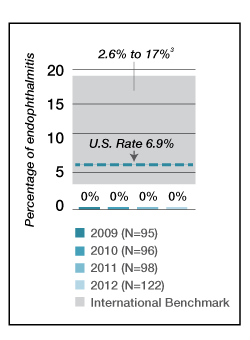
The standard Mass. Eye and Ear protocol for eye trauma has resulted in the lowest civilian endophthalmitis rates – less than 1% of cases – reported in the country.
The literature suggests that endophthalmitis rates around the world range from 2.6% to 17%. The United States National Eye Trauma Registry has reported an endophthalmitis rate of 6.9% after open-globe repair.3
3Andreoli CM, Andreoli MT, Kloek CE, Ahuero AE, Vavvas D, Durand ML. Low rate of endophthalmitis in a large series of open-globe injuries. Am J Ophthalmol 2009; 147(4): 601-608.
Clinical Resources
- Visit www.uptodate.com for a detailed, peer-reviewed, open-globe primary evaluation and management protocol. Search topic: Open-Globe Injuries: Emergent evaluation and initial management
- View Mass. Eye and Ear’s Quality and Outcomes 2013 report
- Find out how Mass. Eye and Ear’s RD-OGI score can help predict risk of retinal detachment after open-globe trauma.