eye Insights Issue 03: The Boston KPro
 eye InsightsTM Issue 3 focuses on the Boston KPro, specifically on how to manage complications associated with implantation, postoperative treatment guidelines, and new clinical innovations.
eye InsightsTM Issue 3 focuses on the Boston KPro, specifically on how to manage complications associated with implantation, postoperative treatment guidelines, and new clinical innovations.
Eye Insights is a clinical newsletter published by Massachusetts Eye and Ear and Massachusetts General Hospital.
“The clinical success of the Boston KPro has required a great collaborative effort among Harvard’s ophthalmic research community and close research partners at MIT. Turning the Boston KPro into a viable, clinical reality for patients has required multi-disciplinary expertise not only in surgery but in biomaterials, bioengineering, optics, inflammation, bacteriology, glaucoma, retinal detachment, plastics and contact lenses.”
– Claes Dohlman, MD, PhD
Inside:
- The Boston KPro: Revolutionized the Field of Corneal Transplantation
- Post-operative Guidelines
- Managing Complications
- Claes Dohlman, MD, PhD: The Father of Modern Corneal Science
- New Innovations and Related Reading
Editor-in-Chief: Joan W. Miller, MD, FARVO
Managing Editor: Matthew F. Gardiner, MD
Communications Director: Suzanne Ward
Scientific Communications Manager: Wendy Chao, PhD
Publications Manager: Wendy Weissner
Clinical Advisory Group: Carolyn E. Kloek, MD, Deeba Husain, MD, Ankoor S. Shah, MD, PhD, Angela V. Turalba, MD
KPro Contributors: Claes Dohlman, MD, PhD, Marlene Durand, MD, James Chodosh, MD, MPH, Roberto Pineda II, MD, Andrea Cruzat, MD, Alja Crnej, MD
Browse all issues > > | Email: eyeinsights@meei.harvard.edu
| eye Insights 3 PDF | 966 KB |
The Boston KPro: Revolutionized the Field of Corneal Transplantation
Dear Colleagues,
Nearly five million people in the world are blind from corneal disease in both eyes, and millions more have corneal blindness in one eye. For some people, conventional corneal transplantation is a successful and life-changing intervention. Many others, however, suffer multiple transplant failures or have corneal conditions that make them poor candidates for traditional transplantation.
Conceptualized at Mass. Eye and Ear in the 1960s by Claes H. Dohlman, MD, PhD, the Boston Keratoprosthesis (KPro) has revolutionized the field of corneal transplantation over the last two decades. Since achieving FDA status in 1992, the Boston KPro has undergone continuous design innovations that have significantly improved the safety and long-term success of the implant. Today, the Boston KPro is the most commonly used corneal prosthesis in the world with more than 11,000 implantations to date in 66 countries by 598 surgeons. In 2014, KPro received European Conformity (CE) mark approval, making the device reimbursable across the European market and, thus, accessible to many more people.
This issue of Eye Insights™ offers treatment guidelines and recommendations from our KPro experts for maximizing the safety and effectiveness of the device, particularly for patients who suffer from glaucoma, autoimmune disorders, and post-operative infections. We hope you find this information useful in your clinical practice. For more information on KPro and our team, please visit MassEyeAndEar.org.

Joan W. Miller, MD, FARVO
Henry Willard Williams Professor of Ophthalmology
Chair, Harvard Medical School Department of Ophthalmology
Chief of Ophthalmology, Massachusetts Eye and Ear and
Massachusetts General Hospital
Recommendations: Boston KPro Follow-up
Advances in postoperative care have greatly improved the clinical success of the Boston KPro. Common complications such as inflammation and infection are significantly lower with today’s prophylactic drug regimens. Innovative devices have also improved postoperative management of KPro. Soft contact lenses are now worn continuously to enhance graft retention, and prevent irritation and evaporative damage.
Prophylactic Antibiotic Regimen
Daily antibiotics are recommended for life and regimens are subject to regional availability, cost and bacterial resistance. Option 1 is preferred at Mass. Eye and Ear. Polytrim™ is presently less expensive than 4th-generation fluoroquinolones. If antibiotics are unavailable, 1% povidone iodine 2 to 4 times daily can be used for the short-term. Patients should be cautioned to avoid eye rubbing, as infectious or toxic debris may be pushed into the eye.
Non-Autoimmune Patients:
- Option 1 - Polymyxin B / Trimethoprim (Polytrim™) 1 x /day
- Option 2 - Fluoroquinolone (4th generation) 1 x /day
- Option 3 - Fluoroquinolone (4th generation) and Vancomycin 1 x /day
Autoimmune or Monocular Patients:
- Option 1 - Polymyxin B / Trimethoprim (Polytrim™) and Vancomycin 1-2 x /day
- Option 2 - Fluoroquinolone (4th generation) and Vancomycin 1 x /day
- Option 3 - Fluoroquinolone (4th generation) and Chloramphenicol 1 x /day
Fungal Prophylaxis
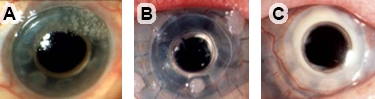
Signs of fungal presence include mulberry shaped deposits on soft contact lens (colonization, figures A and B) and a white sheen around the stem (keratitis infection, figure C). If fungal infection is suspected, discontinue steroids before treating with anti-fungals. Additionally, the contact lens should be replaced if any signs of fungal colonization or infection occur.
- Option 1 - Amphotericin B (0.15%) 2 x / day for 1 week (every 3 months)
- Option 2 - Natamycin (5%)
Corticosteroids
To control inflammation after KPro implantation, prednisolone 1% drops 2-4x per day for the first month are recommended. After the first month, taper to adjust for level of inflammation.
Soft Contact Lenses
After KPro implantation, a large, soft contact lens worn as extended wear is preferable. Contact lenses will need to be worn constantly for life. Lenses can be any Dk and any diameter and curve that fits.
Troubleshooting Common Contact Lens Problems
- If retention is a problem, increase diameter of soft contact lens to 18-22mm or refit with hybrid lens.
- If soft contact lens is clear (no deposits), routine replacement is not necessary. Mass. Eye and Ear recommends cleaning every 3-6 months in the clinic.
- If repeated vision-impairing deposits build up, requiring frequent replacement of the soft contact lens, switch to a hybrid lens (rigid gas permeable center with soft periphery).
- If conjunctival erosion develops over the tube of a glaucoma shunt and not the plate, increase the diameter of the soft contact lens and add Vancomycin drops if on Polytrim™ alone.
- If there is significant mucus associated with the erosion, or if the erosion does not heal in 1-2 months after the soft contact lens change, consider surgical repair.
Glaucoma and Boston KPro
Ideally managed jointly with a glaucoma specialist, the prevention of glaucoma after Boston KPro surgery should be considered a priority at the time of KPro evaluation and during each postoperative visit.
- Prior to KPro Surgery: Consider treating patients with glaucoma with eye drops prophylactically. If glaucoma is diagnosed prior to KPro surgery, consider Ahmed™ valve shunt implantation before, or simultaneously with, KPro implantation. Mass. Eye and Ear recommends creating a long scleral tunnel and placing the tube into the anterior chamber. The tube can also be placed in the pars plana if the patient had a full vitrectomy.
- After KPro Surgery: Target low intraocular pressure—ideally 7 - 15 mmHg by finger palpation, depending on glaucoma stage. Consider performing Ahmed™ valve shunt implantation early if intraocular pressure rises or if the cup to disc ratio increases.
-
Frequency of Tests:
- Intraocular Pressure - Repeat every 3 months
- Cup to Disc Ratio - Repeat every 3 months
- Visual Field - Repeat every 3 months
- Retinal Nerve Fiber Layer Measurement - Repeat every 6 months
- Disc Photos - Repeat every 12 months
Managing Complications
Glaucoma
The diagnosis and follow-up of glaucoma in Boston KPro-implanted patients are complicated because of the difficulty of measuring intraocular pressure accurately with standard tonometers due to the rigidity of the KPro back plate. An alternative is finger palpation of the sclera, though this method can be subjective and only gives an estimate of the pressure. Additional tests for glaucoma, such as visual fields, fundus photography, and optic nerve imaging, are important for the follow-up.
Autoimmunity
Although a small, but important, group of presumed autoimmune diseases (Stevens–Johnson syndrome, mucous membrane pemphigoid, graft-vs-host disease, atopy, uveitis, etc.) have the least favorable outcomes with KPro surgery, these patients also are the most likely to experience failure with standard corneal allograft surgery. Hence, these patients have the most to gain from KPro implantation. The degree of preoperative chronic inflammation may be predictive of postoperative complications. Implantation of the Boston KPro in patients with autoimmune diseases should be performed only in experienced KPro centers.
Infection
Microbial keratitis is characterized by infection of the donor corneal graft, typically around the KPro stem where uncontrolled infectious organisms can access the inside of the eye. Follow-up is essential to recognize infection before endophthalmitis can set in. Endophthalmitis, usually from Gram-positive bacteria, is almost always consecutive to microbial keratitis. Inflammation should be considered infectious until proven otherwise. Microbial endophthalmitis can occur without signs of infection, and should be referred to a vitreoretinal specialist if suspected. Treatment includes vitreous biopsy, intraocular antibiotics, and an antifungal agent, depending on clinical suspicion.
The Father of Modern Corneal Science
Born in 1922 in Sweden, Claes Henrik Dohlman, MD, PhD stands as one of the most highly honored ophthalmologists in the world. Recognized as the founder of modern corneal science, he has produced work that is now considered “classic” literature on understanding corneal biology. His investigations of corneal physiology laid the groundwork for modern clinical practice in dry eye disease, management of corneal burns, wound healing, corneal transplantation, and keratoprosthesis.
Dr. Dohlman’s six decade career reflects many firsts: first in the world to create an organized cornea subspecialty (Mass. Eye and Ear), first to create a formal structured cornea fellowship program (Mass. Eye and Ear and Schepens), first to recruit full-time cornea fellows to Harvard Medical School Department of Ophthalmology, and first to pioneer surgical innovations in keratoplasty and keratoprosthesis. His most notable achievement is the Boston KPro, from which he receives no personal profits.
During his career, Dr. Dohlman has trained first-hand over 200 cornea specialists—more than any other ophthalmologist in the world. His “real” contributions to ophthalmic education are incalculable considering the hundreds of second- and third-generation cornea specialists who have trained under his protégés.
Among his honors are an AAO Laureate Award, the Gullstrand Gold Medal (awarded once every decade), and a named Harvard Professorship. Despite a lifetime of accomplishments, Dr. Dohlman continues to channel his energy into further developing KPro, shaping and setting new standards for the field, and inspiring the ophthalmology and vision research communities.
Innovations and Related Reading
A Revolutionary Technology
 Dr. Claes H. Dohlman’s most notable achievement is the Boston Keratoprosthesis (KPro), a collar button design keratoprosthesis composed of a front plate with a stem, which houses the optical portion of the device, and a back plate with a slit. Available in Type I and Type II designs, the KPro Type II model is reserved for severe end stage dry eye conditions and is similar to the Type I except it has a 2 mm anterior nub designed to penetrate through a tarsorrhaphy.
Dr. Claes H. Dohlman’s most notable achievement is the Boston Keratoprosthesis (KPro), a collar button design keratoprosthesis composed of a front plate with a stem, which houses the optical portion of the device, and a back plate with a slit. Available in Type I and Type II designs, the KPro Type II model is reserved for severe end stage dry eye conditions and is similar to the Type I except it has a 2 mm anterior nub designed to penetrate through a tarsorrhaphy.
A Promising Option for Many
The Boston KPro is now the treatment of choice for a growing list of corneal conditions, and the procedure of choice where corneal transplantation is expected to fail. When managed in experienced KPro centers, the prosthesis also can be a life-changing intervention in patients who have suffered severe chemical injuries and blinding autoimmune disorders.
KPro Around the Globe
 Despite millions of people requiring corneal transplants, there is a widespread lack of eyebanks and suitable donor tissues, especially in developing countries. KPro team members, James Chodosh, MD, MPH and Roberto Pineda II, MD are working to make the KPro available to some of the world’s poorest areas and have taught surgical implantation techniques and follow-up care to ophthalmologists and medical staff around the globe. Dr. Pineda has helped to establish self-sustaining KPro clinics in developing countries, including India, Thailand, Sudan and Ethiopia, while Dr. Chodosh is working on developing a low-cost KPro to help bring its sight-saving benefits to these populations.
Despite millions of people requiring corneal transplants, there is a widespread lack of eyebanks and suitable donor tissues, especially in developing countries. KPro team members, James Chodosh, MD, MPH and Roberto Pineda II, MD are working to make the KPro available to some of the world’s poorest areas and have taught surgical implantation techniques and follow-up care to ophthalmologists and medical staff around the globe. Dr. Pineda has helped to establish self-sustaining KPro clinics in developing countries, including India, Thailand, Sudan and Ethiopia, while Dr. Chodosh is working on developing a low-cost KPro to help bring its sight-saving benefits to these populations.
New Innovations
Current research efforts led by Eleftherios Paschalis, PhD, focus on improving KPro’s aesthetics by coloring the titanium back plate blue or brown. Collagen crosslinking, provided as part of a clinical trial at Mass. Eye and Ear led by Joseph Ciolino, MD, is also helping to strengthen the ocular tissue around the KPro and help maintain the prosthesis better. Furthermore, Dr. Ciolino and colleagues from Boston Children’s Hospital and Massachusetts Institute of Technology have developed a drug-eluting contact lens, which could improve surgical outcomes for patients with KPro by both protecting the ocular surface of the eye and by preventing postoperative infections. One day, these lenses may replace eye drops.
RELATED READING
- Aldave AJ, et al. International results with the Boston Type I Keratoprosthesis. Ophthalmology. 2012 Aug;119(8):1530-8.
- Ciolino JB, et al. Retention or the Boston Keratoprosthesis Type 1. multicenter study results. Boston Keratoprosthesis Type I Study Group. Ophthalmology 2013; 120:1195-2000.
- Srikumaran D, et al. Long-term outcomes of Boston Type I Keratoprosthesis implantation: a retrospective multicenter cohort. Ophthalmology 2014;121(11):2159-64.
- Crnej A, et al. Glaucoma progression and role of glaucoma in patients with Boston keratoprosthesis. Cornea 2014;33(4):349-54.
